Cancer is often talked about as if it’s a single disease, with a single, elusive cure. The reality is that cancer is not a single disease. In fact, tumours are as unique as the patients who carry them. To make matters worse, cancer can be a moving target, that evolves in response to treatment. These vexing aspects of cancer are widely recognized by cancer researchers and many patients, but not by many outsiders.
Today, I want to help you understand cancer from the inside out, and shed light on why it’s such a formidable foe. Let’s start at the beginning, with the causes of cancer.

What causes cancer?
Cancer is a disease in which some of the body’s cells grow uncontrollably and can spread to other parts of the body. This uncontrolled growth is caused by genetic (DNA) mutations in cancer-causing genes, paired with a failure of our bodies to clear out abnormal cells.
Cancer-causing DNA mutations can happen for several different reasons. They can be inherited from our parents, like BRCA1 mutations that increase our risk of developing breast and ovarian cancer. They can be due to factors that damage our DNA, such as the chemicals in tobacco, or UV rays from the sun. Or, they can simply be due to errors in the normal process of cellular division and growth. Every day, trillions of cells in your body are replicating and dividing; each division is an opportunity for a small mistake with big consequences.
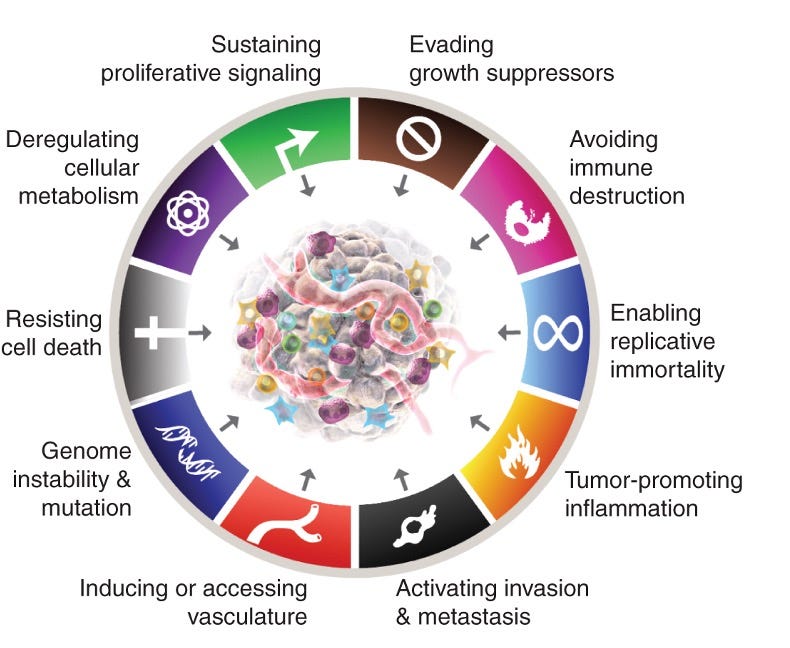
Researchers believe that there are ten major ways that normal cells become tumours, often referred to as the "Hallmarks of Cancer". These “hallmarks” include mechanisms like enabling replicative immortality (dividing infinitely), resisting cell death, and avoiding immune destruction. This landmark paper was first presented by Bob Weinburg and Doug Hanahan in 2000, updated in 2011, and revised in 2022. The most recent version is shown here:
Every tumour is unique
While cancers can be broadly described using the ten hallmarks shown above, there are many different ways for tumours to realize each of these hallmarks. So far, scientists have identified a staggering 719 cancer-related genes according to a 2018 study called the Catalogue of Somatic Mutations in Cancer (COSMIC) Cancer Gene Census (CGC). Any given tumour will have some subset of these 719 cancer-related mutations, which promote cancer through the 10 hallmarks described above. The figure below shows how a gene called PTEN both promotes and suppresses cancer hallmarks.

The complexity of cancer goes even deeper than this: it’s not unusual for the same patient to have different mutations within various parts of the same tumour. This occurs because DNA mutations can lead to even more mutations, especially when initial mutations affect our internal error-checking systems.
Cancers can evolve
In the same way that bacteria evolve to evade antibiotics and viruses evolve to evade anti-virals, tumours can evolve to evade a cancer drug. Tumour resistance is a massive challenge for cancer therapies, and is a major cause of cancer-related deaths.
At the heart of tumour resistance is the heterogeneity and plasticity of tumours. For example, patients treated with erlotinib, a drug used in EGFR+ non–small cell lung cancer (NSCLC), can become drug resistant when the tumour develops mutations in the drug target (EGFR). Drug resistance to cancer drugs can also evolve in many other ways, such as through cellular changes that bypass a pathway that a drug acts to suppress. Research is ongoing into strategies to avoid or overcome the many different causes of treatment resistance.
Looking forward
Today, we’ve taken a deep dive inside cancer cells to understand them from the inside out. We’ve looked at the causes of cancer, the diversity of cancers, and the plasticity of cancers. We’ve only scratched the surface on each of these topics, but I hope you can begin to appreciate why cancer is such a formidable foe.
Asking for a single cure for cancer is asking for a single cure for blindness, deafness, arthritis, or any other disease with many causal pathways. It's hard to imagine how a single drug could address all "flavours" of cancer. If anyone ever tells you they have a universal cure for cancer, this is a huge red flag. Sorry, Big Pharma is not keeping it a secret!
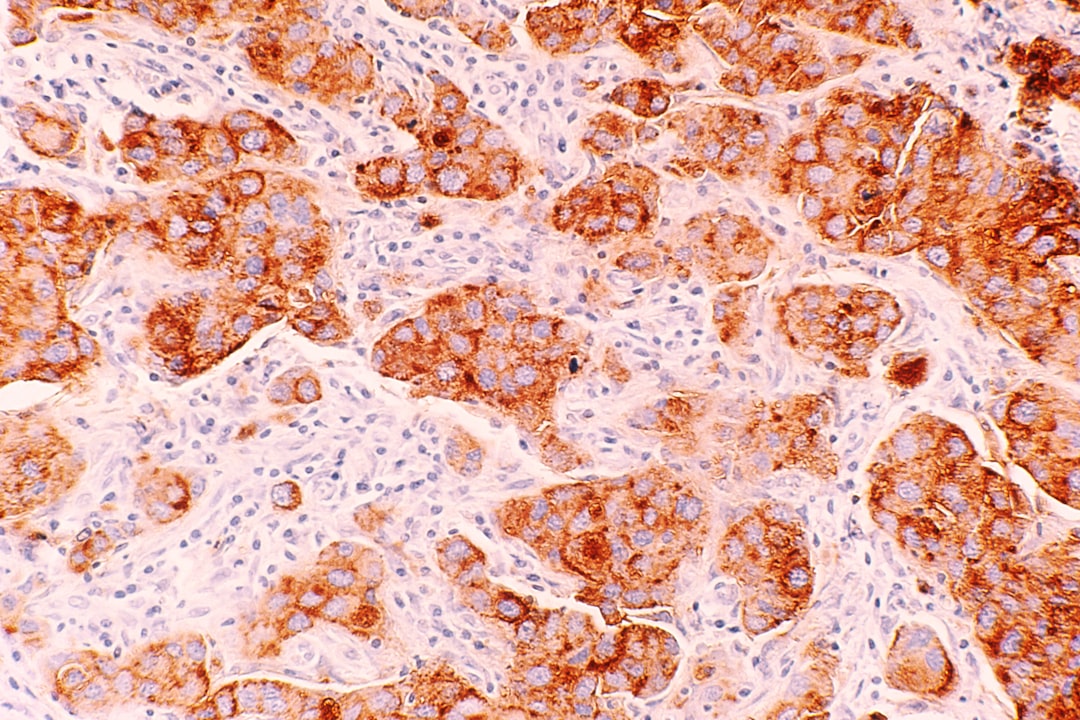
At the same time, I’m truly optimistic about the future of cancer treatments. Scientists are continually unlocking the molecular secrets of cancer, discovering new therapeutic strategies, and finding ways to tackle drug resistance. Several decades ago, the era of targeted therapies (personalized or precision medicine) began, with the development of therapies that target the Achilles heel of a tumour. We now have a growing array of highly effective targeted drugs - like Imatinib/Gleevec for chronic myelogenous leukemia (CML) and trastuzumab/Herceptin for HER2+ breast cancers. Indeed, researchers and clinicians are increasingly categorizing - and treating - tumours based on their underlying cause and molecular “flavour” in addition to their anatomic site. For example, some gastric cancers are treatable with trastuzumab (Herceptin) - the drug originally developed for HER2+ breast cancer - because they share a similar molecular fingerprint (HER2+). More recently, cancer immunotherapy, which harnesses the immune system to defeat cancers, has matured to the point where it is becoming a key part of our cancer-fighting toolkit. Several approved treatments are being used regularly, and many promising forms of cancer immunotherapy are under development, including oncolytic virus therapies, cancer vaccines, cytokine therapies, adoptive cell transfer, and immune checkpoint inhibitors.
Closing thoughts
It would be wonderful to find a cure for all cancers, but this is simply not realistic. Ultimately, we need a menu of treatments and strategies that fit the unique needs of each patient, and can respond to the evolving nature of tumours. This is a lofty goal, but one that I believe is attainable, as we continue to deepen our understanding of cancer.
Regardless of our treatment arsenal, prevention and early detection will always the best strategy for defeating cancer. Perhaps a topic for a future post?
Warm regards,
Learn More
What is cancer? (National Cancer Institutes)
What causes cancer? (Cancer Research UK)
Cancer.Net – Oncologist-approved information about cancer (by American Society of Clinical Oncologists)
Related Podcast Episodes
Get Real Health with Dr. Chana Davis (Ep 52). Understanding Breast Cancer with with Dr. Stephanie Graff. Available my website, Apple Podcast or Spotify.
Personal Notes
I am not a cancer survivor, but do have a deep scientific appreciation for the diversity of cancer, and the implications for cancer detection and treatment. During my PhD, I studied genetics as Stanford in the lab of Pat Brown, one of the inventors of DNA microarrays. This new tool was being used to unravel new molecular "flavours" of cancer, and reshape the way the disease was defined. I then spent several years working in cancer early detection at the Canary Foundation, where it was clear that each disease (ovarian cancer) had many diseases within it, that will require different detection approaches. Later, I worked in the oncology companion diagnostics group of Genentech/Roche, where our mission was to guide cancer treatments towards those who were most likely to benefit, using molecular tools to study tumours.



